Cancer patients are getting younger. Mays Cancer Center experts explain the modern factors at play


More people under the age of 50 are facing cancer diagnoses today compared to the same age group in the 1990s. A report from the American Cancer Society released earlier this year states that while cancer deaths are on the decline, the number of overall cases is rising and expected to hit a high of 2 million for the first time in a single year.
David Gius, MD, PhD, is a professor and assistant dean of research at The University of Texas Health Science Center at San Antonio. He studies aging and cancer — particularly breast cancer — and serves as the associate director for translational research at the Mays Cancer Center at UT Health San Antonio.
“Age and aging are words commonly used but never rigorously defined. And we don't do that in medicine either,” Gius said.
Aging is qualitative. Gius explained a doctor might write in their notes that a patient appears younger or older than their stated age. This is not unsimilar from an acquaintance saying you “look” young for your age.
“That's strictly a descriptive characterization of someone. Aging is a descriptive quality assessment that we make — not based on any real rigorous quantitative measurements,” he said.
Longevity, however, is quantitative and refers to how long a person is expected to live. That number isn’t static; rather, it can grow with you.
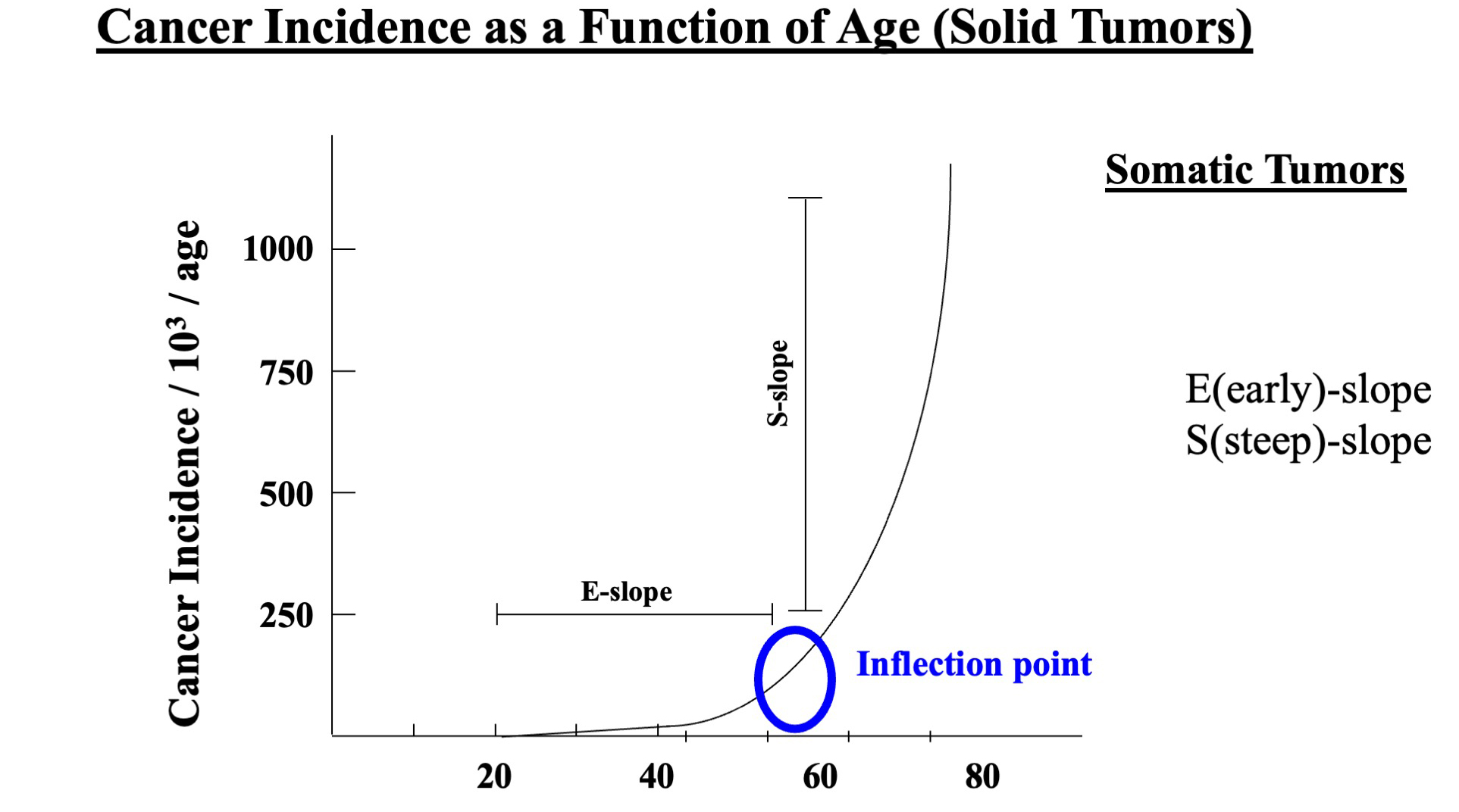
However, when a person turns about 50, the risk of aging-related diseases sharply increases. This includes cardiovascular disease, type 2 diabetes, neurologic/neurodegenerative diseases and cancer.
Modern environmental factors at play
Why then are so many people under the age of 50 getting cancer right now?
“Cancers in young people are surprisingly increasing. No one knows why. And that's probably either heritable or environmental,” Gius says. “It's probably not biological.”
Environmental factors relate to diet, exercise and other lifestyle variables.
Colorectal cancer, for example, is especially increasing among young Americans as the no.1 and no. 2 cancer-related deaths for men and women under 50 respectively. Its risk factors are both heritable and environmental.
Lakshmi “Bala” Balasubramanian, MD, MS, is an associate professor in the Division of Hematology-Oncology at UT Health San Antonio and a gastrointestinal medical oncologist at Mays Cancer Center.
“In the past 30 years, we've seen a doubling of cancer rates in younger individuals, and it likely is a combination of a mixture of many of these Western world modernization problems with processed foods, not getting enough exercise, red meat consumption and gut microbiome changes with the antibiotic uses,” she said.
Experts have also seen climate change playing a role in cancer-related risk factors, especially in Texas. Bala paints this picture as an example: Texans were stuck in a heat dome for several months, and as a result, even nighttime temperatures increased by two degrees on average which did not allow for cooling to happen.
“And the easiest form of exercise we can pursue, which is walking, is taken away from us or limited,” she said.
This also creates a domino effect, especially for the most vulnerable.
“So, people are trying to cool their hot homes with an increased cost of cooling, trying to decide whether they pay their electricity bills, fix a broken AC, pay their medical bills, buy healthy affordable food, or get a gym membership to exercise,” she said.
“They’re all competing threat multipliers to being healthy.”
Solutions to look toward
While these compounding factors may create a bleak outlook, there are possible solutions at a national and individual level.
A recent change from the Environmental Protection Agency limits industries more strictly on the amount of air pollution, or particulate matter, they are allowed to emit from 12 micrograms per cubic meter of air to nine. Decreasing air pollution is known to help decrease the risk for breast and lung cancer.
Additionally, the Montreal protocol, an international agreement to cease production of certain ozone depleting hydrofluorocarbons, including freon, is helping to close the hole in the ozone layer, decreasing the risk of skin cancer by lessening the exposure for UV rays.
Bala said future, more stringent policy changes with environmental factors in mind may look toward regenerative farming; and at the healthcare level, should continue to include stool testing and colonoscopy screening as part of basic inclusive coverage starting at age 45.
At the personal level, farmers markets and container gardens can be accessible and inexpensive options to decrease cancer risk factors.
By discovering the fruits and vegetables that have the highest exposure of pesticides and substituting those products for organic versions or growing your own — you can “put your money where it matters,” Bala explains. This can include berries, peppers, beans and herbs.
When it comes to exercise, implementing a buddy system can be helpful, especially for those who live in urban areas. Walking in parks or playing recreational sports are impactful ways to get physical activity and social interaction.
And while environmental factors include what you expose yourself to — healthy diet and exercise — it also includes what you don’t expose yourself to.
“Some people think an increase in cancer is because of the improvement in public health initiatives. For instance, we don't play in the dirt anymore. That's probably a bad thing because dirt has all these antigens that children get exposed to,” Gius said.
It is ironic that in the last century, pollution has made the planet less clean, or rather green, while the people who make up its population are generally cleaner, and public places more sanitized — which has created a deficit in adaptive immunity.
Prevention before treatment
Gius says one problem of medicine in America is the disproportionate focus on cancer treatment versus prevention — partly because of how big the U.S. is and how many people are in it.
New discoveries in treatment are undoubtedly helping save lives, but a lack of surveillance and prevention still allows many people to slip through the cracks. Screening, particularly for colorectal cancers, is increasingly important for people when they turn 45 — and even younger if they have a family history or other risk factors.
The first step toward improving prevention efforts will likely require a society shift in understanding that cancer risk factors — including climate change, lack of exercise, increased exposure to processed foods and financial toxicity — are essential health issues that must be addressed.

 Close
Close