

Breast Cancer Reconstruction
Breast reconstruction surgery at Mays Cancer Center
When you choose us, you receive care from highly experienced, fellowship-trained plastic and reconstructive surgeons specializing in breast reconstruction. They are part of a multidisciplinary team working to deliver personalized care and excellent outcomes.
Patients put their trust in our team because we consistently help women attain breasts with a natural look and feel. We explain what to expect and help you make the right decision for your needs.
We offer all available options for immediate and delayed reconstruction using implants, flaps and oncoplastic breast cancer surgery techniques. You are a candidate for breast reconstruction if you have surgery to remove the entire breast (mastectomy) or part of your breast (lumpectomy or partial mastectomy).
Our team tailors services based on your personal preference, cancer diagnosis, body shape, prior surgeries and health history. At your appointment, we discuss your preferences and what to expect. To get started, read our answers to frequently asked questions.
Breast Reconstruction Frequently Asked Questions
What is breast reconstruction?
Breast reconstruction includes a variety of techniques to restore your breasts after surgery for the treatment of breast cancer. It involves added surgery to create new breasts using tissue from your own body, breast implants or both.
There are several options for breast reconstruction, both after a lumpectomy and mastectomy, using implants, flaps or rearrangement of the breast tissue.
The decision to proceed with the reconstruction immediately or delayed is very much dependent on your personalized cancer treatment plan and your overall health. It is our top priority to treat your cancer effectively while providing you with a highly satisfactory reconstructive result.
Is breast cancer reconstruction right for me?
Breast reconstruction can restore a natural-looking appearance and your self-confidence. It offers a permanent solution and alternative to wearing a prosthetic bra. Surgery will also help reduce asymmetry between the breasts that can occur after cancer surgery.
What happens at my first meeting with the surgeon?
Generally, you will see your plastic surgeon after seeing your breast surgical oncologist. This way, your cancer treatment plan has been decided.
At the first visit, your plastic surgeon will perform a breast examination and discuss reconstructive options, taking into account how your breast cancer will be removed (either with a lumpectomy or mastectomy), your health history, including prior surgeries or other medical conditions and if you will need chemotherapy or radiation therapy.
You are welcome to bring a friend or family member to your appointments. This person can help you remember everything we discuss so it’s a little easier to make decisions.
What are my options if I need a mastectomy?
Tissue flap reconstruction
Breast reconstruction using tissue from your own body to re-create a breast provides the most natural result of any technique. The choice of tissue to be moved from another part of your body to your chest to re-create a breast mound will vary, depending on the blood vessels that supply the tissue and the skills of your surgeon.
If a flap-based procedure is right for you, options may include:
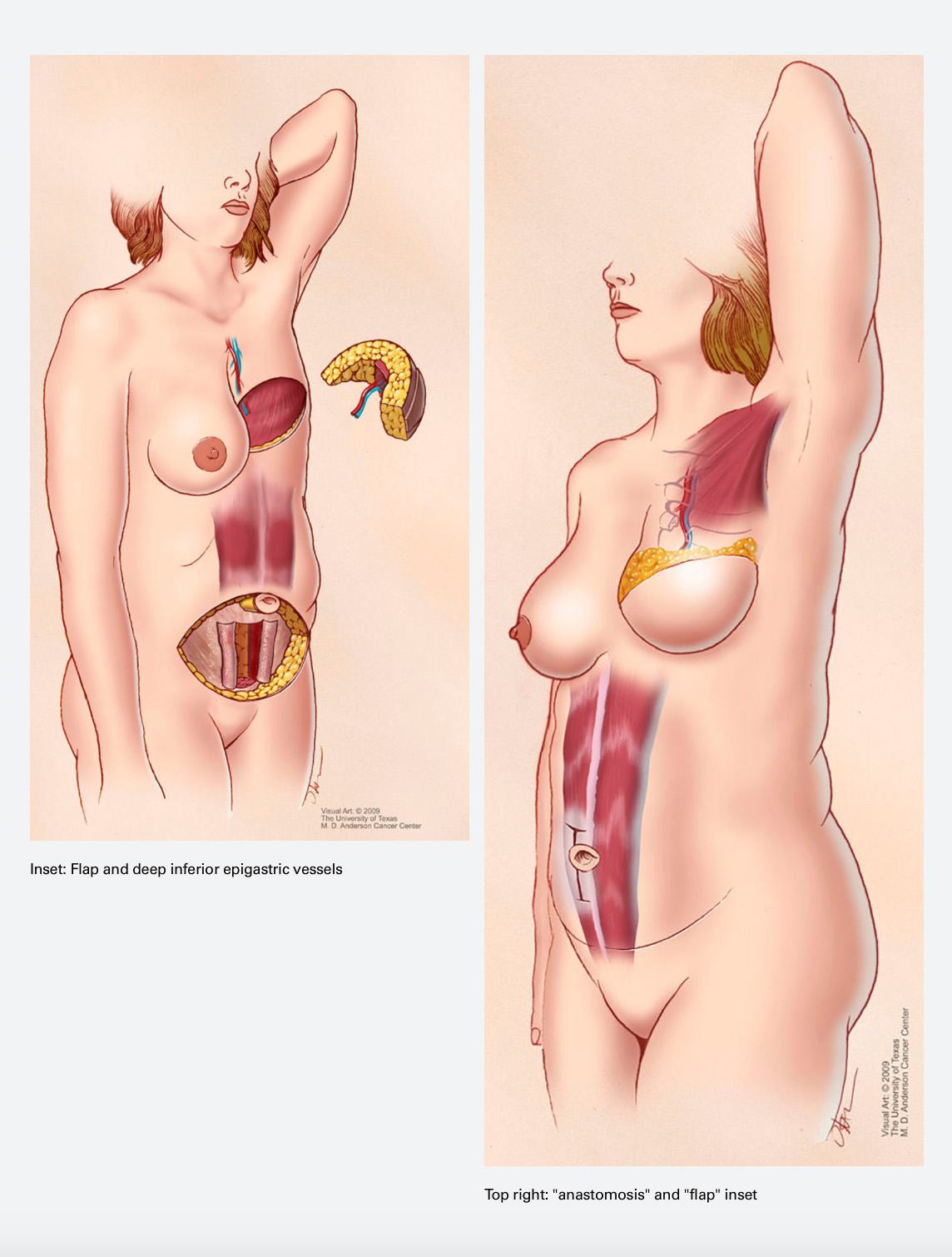
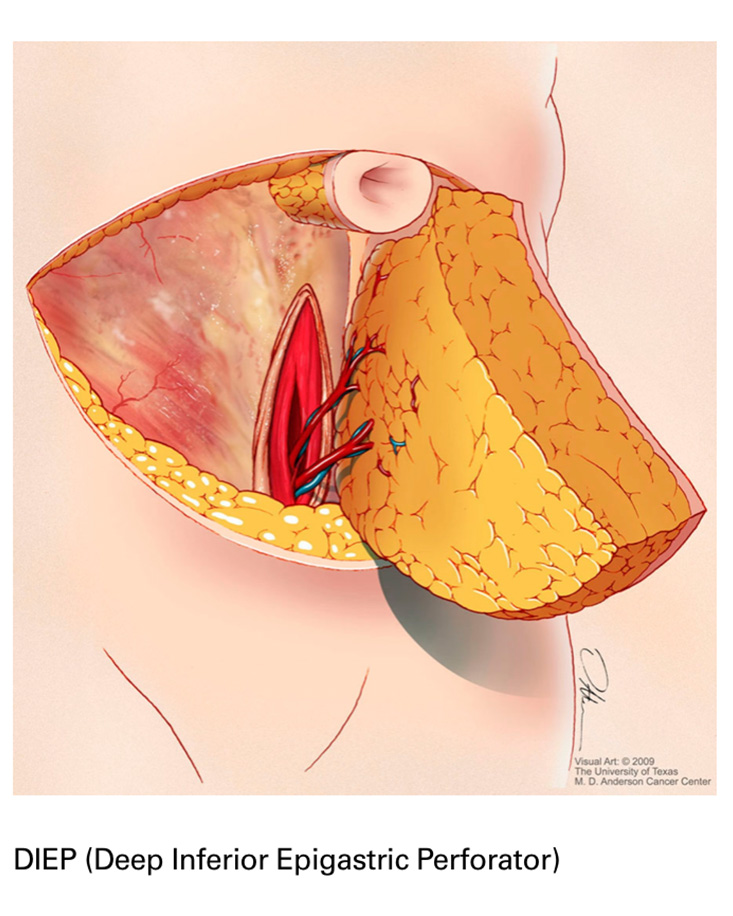
Abdominal free flap: This option is also known as a DIEP (deep inferior epigastric perforator) flap reconstruction. Surgeons may take skin, fat and muscle tissue from your lower abdomen. We transfer the flap and its blood supply to your chest, then reshape and attach it to a nearby artery and vein. This technique typically provides the largest amount of tissue and is the most breast-like in feeling. It is sometimes possible to connect sensory nerves to improve sensation.
Copyright held by, and used with the permission of, The Board of Regents of the University of Texas System through The University of Texas MD Anderson Cancer Center.
- Thigh-based flap: This technique may be an option when an abdominal flap is not possible, most commonly if you have undergone a large abdominal surgery in the past. We may use a transverse upper gracilis flap (TUG), which involves a small muscle from the upper thigh, blood vessels, fat and skin. The profunda artery perforator (PAP) flap uses tissue from the back of the thigh but leaves nearby muscles intact.
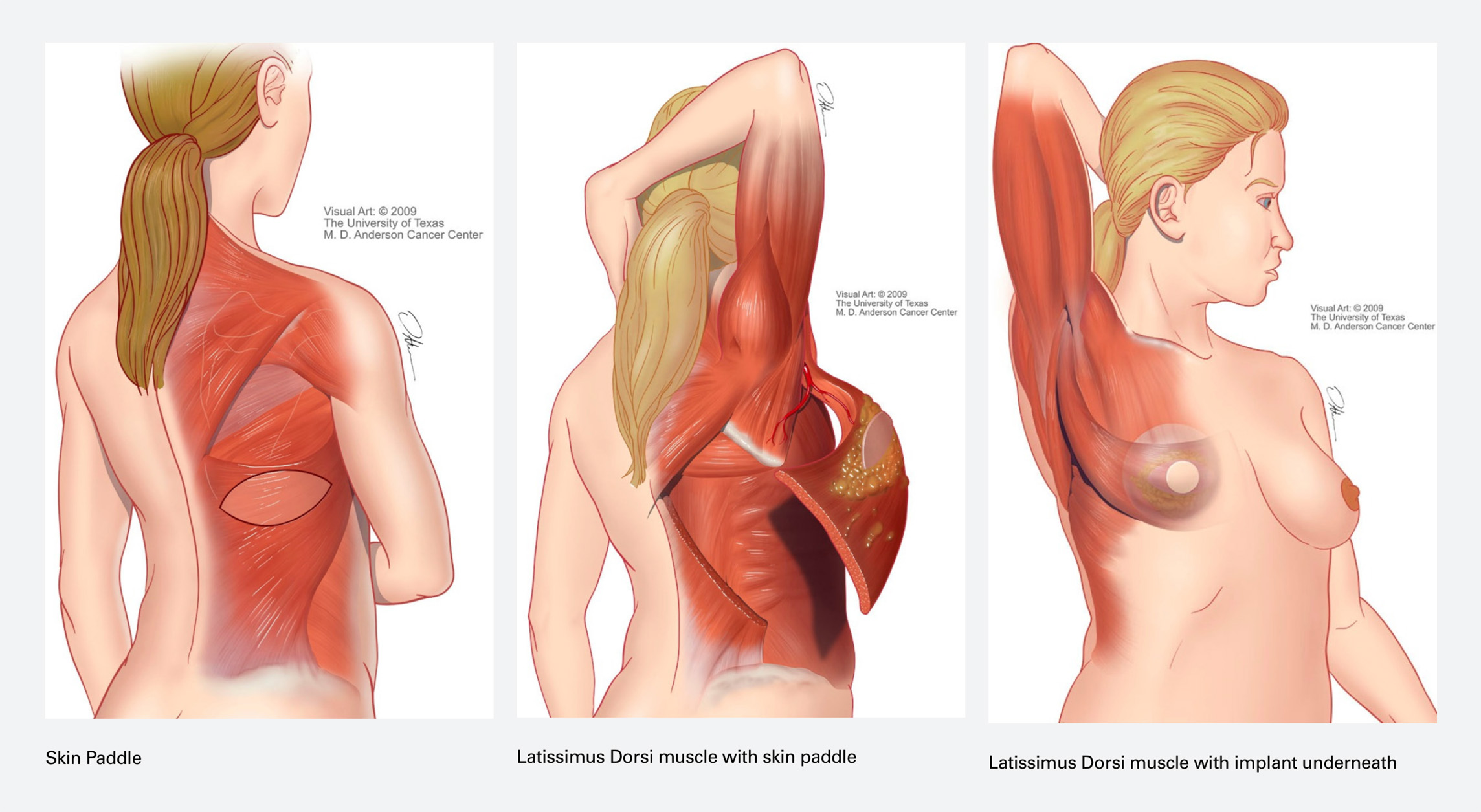
- Latissimus dorsi (LD) flap: Surgeons make an incision on your back near the bra line and isolate a section of fat, muscle and skin. They do not remove the flap from its blood supply. Instead, they slide it past nearby tissue to reach the chest. We may use this option by itself to create a small breast. To create a larger breast, we may use this type of flap in conjunction with an implant
Implants
Implant-based reconstruction does not use tissue from another part of the body. There are two types of implants: saline-filled and silicone gel-filled. Both types of implants have a silicone outer shell. They vary in shape (contour), size and profile. The U.S. Food and Drug Administration has ruled these options as safe and effective. Your surgeon will help determine which implant is best for your body shape.
Implant-based options we offer include:
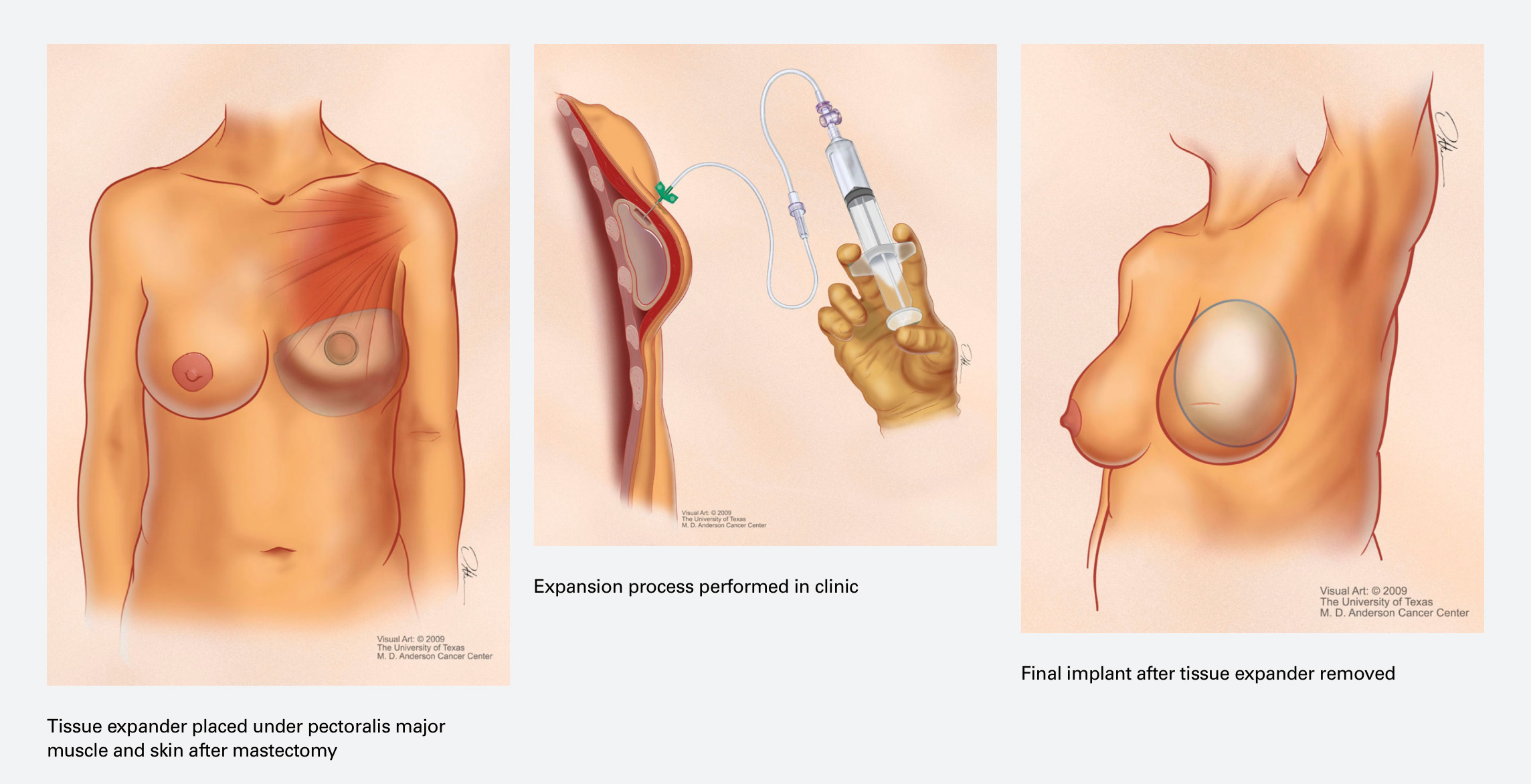
- Skin expansion and implants: We perform a procedure to implant an inflatable device into the breast area. During outpatient visits, we fill the balloon with a saltwater solution, which expands the skin, creating space for a future permanent implant. We remove the device and replace it with a permanent breast implant during a later procedure.
- Direct to implant: Some patients are candidates for placement of permanent breast implants during the same procedure as their mastectomy.
- Flap reconstruction using an added implant: We create a new breast using a flap of skin and fat from another body area, with a permanent implant included to increase the size of the final breast created.
Images via MD Anderson
Additional procedures
Following the main surgeries for breast reconstruction, you may want to undergo additional minor procedures to optimize the shape and appearance of your breasts. They include:
- Nipple reconstruction: Surgeons use nearby tissue to create a new realistic nipple to replace what had been removed during your mastectomy.
- 3D nipple and areola tattooing: We use medical-grade tattooing techniques to create a 3D nipple and areola. This can be done after nipple reconstruction or on its own without nipple surgery if the patient does not want a new nipple bud.
- Symmetry procedures: An additional smaller surgery may be necessary to ensure breasts are of similar shape, size and positioning on your chest. Commonly, this is needed if one breast was reconstructed and the other did not undergo surgery for the treatment of cancer. There are many options, but they include breast lifts (mastopexies), augmentation (implant placement), breast reductions and fat grafting.
What types of breast reconstruction are available after lumpectomy (partial mastectomy)?
You may be eligible for immediate reconstruction using oncoplastic breast cancer surgery. The breast surgical oncologist removes the cancer and the plastic surgeon rearranges the remaining breast to restore its shape and appearance in one procedure. You may still need radiation therapy after surgery since this technique preserves much of the normal breast tissue after the cancer is removed.
The other option is delayed reconstruction. You undergo the lumpectomy procedure and then wait to have reconstruction. There are several options, but the most common surgery for delayed reconstruction is fat grafting. In this surgery, fat is harvested from another part of your body with liposuction and transferred to the breast to correct the lumpectomy defect.
Whether it’s a few months or a few years between lumpectomy and reconstruction, it’s still possible to achieve the look and feel you desire.
Who covers the cost of reconstructive surgery?
Insurance typically covers reconstruction for the breast affected by cancer. It’s part of the Women’s Health and Cancer Rights Act, which mandates the availability of reconstructive surgery following mastectomy.
Insurance also covers efforts to make sure both breasts have a consistent appearance, even if one is cancer-free. We explain how your specific coverage works and whether there will be out-of-pocket expenses.

 Close
Close